Today is Overdose Awareness Day, and End Hep C SF is taking the time to remember our friends, partners, and participants who we have lost to overdose, and to celebrate all the lives we have saved thanks to the DOPE Project and our team of harm reduction warriors in San Francisco. One such warrior is Pauli Gray, an End Hep C SF Coordinating Committee member and leader, and longtime DOPE Project trainer. In this post Pauli reflects on the ways that overdose prevention and HCV services strengthen and support each other, and promote offering both simultaneously.
Today is Overdose Awareness Day, and End Hep C SF is taking the time to remember our friends, partners, and participants who we have lost to overdose, and to celebrate all the lives we have saved thanks to the DOPE Project and our team of harm reduction warriors in San Francisco. One such warrior is Pauli Gray, an End Hep C SF Coordinating Committee member and leader, and longtime DOPE Project trainer. In this post Pauli reflects on the ways that overdose prevention and HCV services strengthen and support each other, and promote offering both simultaneously.
Tell us about the 6th Street Harm Reduction Center. What services do you offer there?
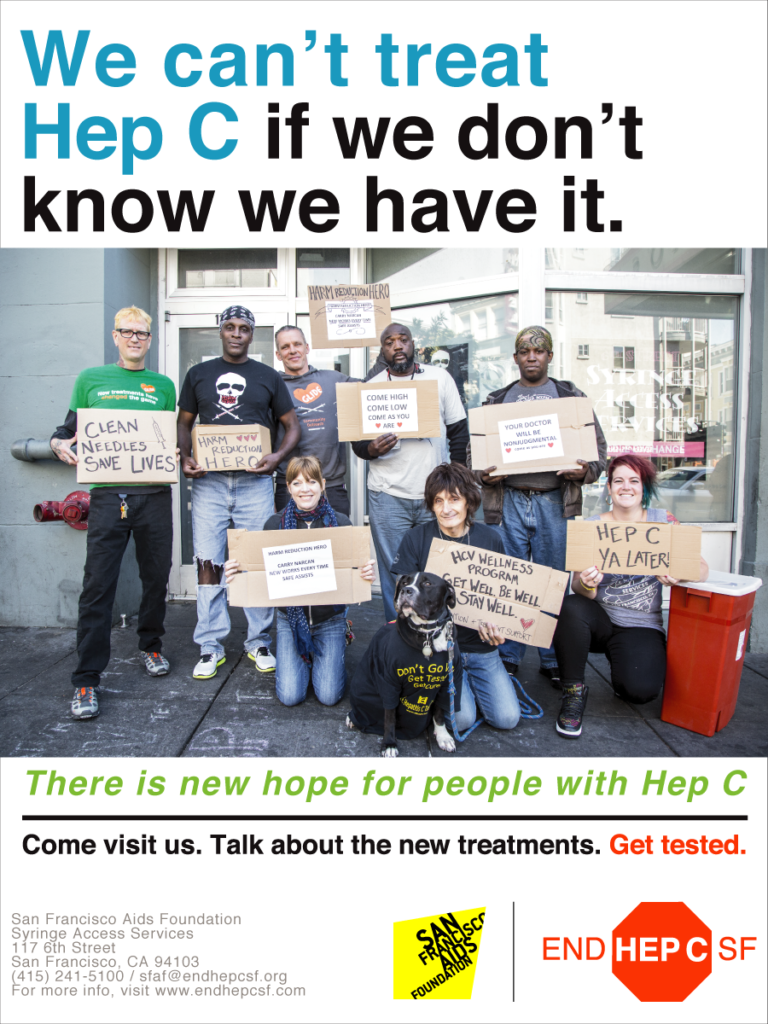
The 6th Street Harm Reduction Center is open 54 hours a week in the South of Market Neighborhood. We offer HIV and hepatitis C testing and linkage to care, health education and therapy groups, overdose prevention training and naloxone distribution, substance use treatment, mental health counseling, low-barrier medical care, and so much more. To accomplish this we partner with the Stonewall Project, the Harm Reduction Therapy Center, Glide Harm Reduction Services, The Dope Project, Street Outreach Services and the Department of Public Health. We are a place of welcome. For many, we are a bridge to improved health and healing.
In terms of our HCV services, we do most of our HCV treatment at our weekly HCV group, which serves good food and tends to be packed each week. For many drug users, getting treated at a syringe access program is the only option for accessing the HCV cure. There is a family unit feel to the HCV program, where clients who have been cured come back every week to help new people and volunteer at group. This month we’ll be formalizing their roles with our new HCV Peer Linkage Program in partnership with End Hep C SF.
We also have wrap around services during, and immediately after group to support our folks living with HCV. These include Hep A and B vaccines, PrEP initiation, HRTC Substance Use/Mental health counseling, Suboxone, wound care and more. We are constantly providing overdose prevention and response trainings and distributing naloxone. We provide lockers for homeless and chaotic clients to store HCV meds and antibiotics, which really helps support their success.
How do you think being a DOPE trainer helped prepare you to do quality HCV linkage work with drug users?
I started as a DOPE Trainer in 2004. It has helped me immensely as a HCV Care provider and planner because it reminded me constantly that our people, our participants, do care deeply about each other. And it also showed me that they care about themselves and how important it is to share that, and to remind them of that. It showed that we can create a space between us to do something positive for the greater good—for other drug users and people in general. Being a DOPE trainer gave me steady practice in having productive and lifesaving conversations, and seeing how these conversations lead to productive and lifesaving actions.
Tell us about why it’s so important to do overdose prevention and HCV testing, linkage, and treatment work simultaneously.
It’s especially important to me because in my world and program, we offer overdose prevention and HCV services in the same place. We offer them where clients are already coming—the syringe access/harm reduction programs. I am a staunch advocate of meeting clients where they’re at physically, not just as a theory. These are the two main lifesaving and changing things we can do for what I consider my people, and they should be done together. Each service can provide an entry to the other, and the services support and strengthen each other.
Are there ways that your clients talk about overdose prevention and HCV work similarly or differently? How so?
Overdose prevention is for everyone who accesses our services—they generally need the same information and tools. HCV conversations depend on a person’s situation and status. Does this person need treatment themselves? Have they been tested? Should we focus on safer injection/prevention counseling? Do they need basic information to pass on to their friends so their friends can be cured? We figure out where folks are in the continuum and we work from there.
Is there an overdose prevention and/or HCV cure success story you’d like to share?
I have many. When I’m doing Narcan/OD response trainings I am already in the process of learning a person’s story and developing trust between us. After we create that bond during an overdose prevention training, it’s easy to shift our conversation to discussing HCV.
One overdose prevention client was a female who had visible bruises when I first met her. She developed trust in me from the conversation about overdose prevention and wanted to pursue HCV treatment with me when I offered it. It turned out she was in an abusive relationship and wanted to get herself into a safer situation. She decided she wanted to start opiate substitution therapy before starting the HCV treatment process. We ended up doing both these things and she is currently one of the peer leaders of my program. AND she is happily married to another HCV client. There are lots more equally inspiring stories coming out of our HCV program at the 6th Street Harm Reduction Center, and many of them start with overdose prevention trainings.
We’re so grateful to be able to offer clients a variety of options and supports to help them set goals and make positive changes. Part of our program is a Secondary Goal initiative: participants feel so much better after just a month of HCV TX that they set other goals like managing or even stopping drug use, volunteering, employment, reuniting with families. We urge folks to give back in any way possible as part of the process, and that involves getting naloxone and being vigilant and ready to save others from accidental overdose.
It is also so important to remember that the people treat for HCV, and their partners and friends, remain at risk of overdose. We continually do reinfection prevention counseling AND overdose prevention counseling after they are cured.
Pauli Gray is the Senior HCV Coordinator/Harm Reduction Specialist at the San Francisco AIDS Foundation, where he has worked for twenty years. He is also a member of the End Hep C SF Coordinating Committee, Prevention Testing and Linkage group, and Treatment Access groups. Pauli has dedicated his life to harm reduction, overdose prevention, and curing people of HCV in San Francisco and around the world. He has attended speaking events in Africa, Ukraine, and throughout California. He was awarded the California Society of Addiction Medicine Community Service award last night (August 30th, 2018).